Ashley Fry, a doctor of nursing practice student on the health policy track in the George Washington University School of Nursing, doesn’t limit herself to academic study of her field. A working nurse practitioner in palliative care, Fry also fights to educate legislators in her home state of Colorado about the limitations of current laws for terminal patients—how people facing the end of their lives can maintain their dignity and choose their own path forward.
(Content warning: This Q & A includes discussions of terminal illness and medical aid in dying.)
What is your lobbying work about?
I am educating legislators about the barriers to accessing the resources needed in order to participate in medical aid in dying in Colorado. Medical aid in dying (MAID) is one term used to describe the medical practice by which a terminally ill adult, who has medical decision-making capacity, and a prognosis of six months or less [to live] can choose to obtain prescription medication from their medical provider in order to peacefully end their life. There are currently 10 states, plus Washington D.C., that have legalized this process. The process to obtain MAID varies slightly from state to state.
In Colorado, two physicians must certify the terminal illness and the prognosis, two verbal requests must be made to the attending physician separated by at least 15 days and a written request must also be submitted that is witnessed by two qualifying individuals. Additionally, physicians and health care systems can choose to opt out, and we’ve seen that the religiously affiliated health care organizations are blocking their physicians from participating. The result has been that patients are routinely reporting to me that 1) It is taking them months to find two physicians who are willing to participate, 2) they become too debilitated to continue seeking resources or they die before they can secure those resources or 3) they choose to not even attempt to start the process because it sounds too complicated.
What I am proposing to legislators is that we consider amending our law to look like New Mexico’s End-of-Life Options Act. New Mexico’s law is quite innovative: it allows advanced practice providers—including nurse practitioners, clinical nurse specialist, and physician assistants—to work with a physician to be one of the certifiers of terminal illness. They have reduced their waiting period for obtaining medications from 15 days down to 48 hours, which is particularly helpful to patients since it may take months to find the participating providers.
Finally, those already enrolled in hospice [in New Mexico] have already been declared terminally ill with a prognosis of six months or less. So only one physician, the hospice medical director, needs to certify terminal illness to prescribe MAID medications. If we could amend our law to look more similar to New Mexico’s law, it would help reduce some of the barriers our terminally ill patients who are interested in MAID are facing.
Who are you lobbying and why?
I am working to educate as many state legislators as I can, regardless of party affiliation. I have reached out to legislators from all over the state to build awareness. In particular, our rural legislators will be important in representing their communities. Seventy-seven percent of Colorado’s landmass is rural. We know on the eastern and southern portions of the state in particular, advanced practice providers are serving these communities—there are counties where no active physician is identified and others where advanced practice providers are outnumbering all physicians. If we want to create equitable access to the resources needed in order to participate in the MAID process per the requirements of the law, then we need to take into account the rural health care landscape of Colorado and allow advanced practice providers to be a bigger part of the process.
When did you start working with state legislators on this initiative? Are there other groups involved in this effort?
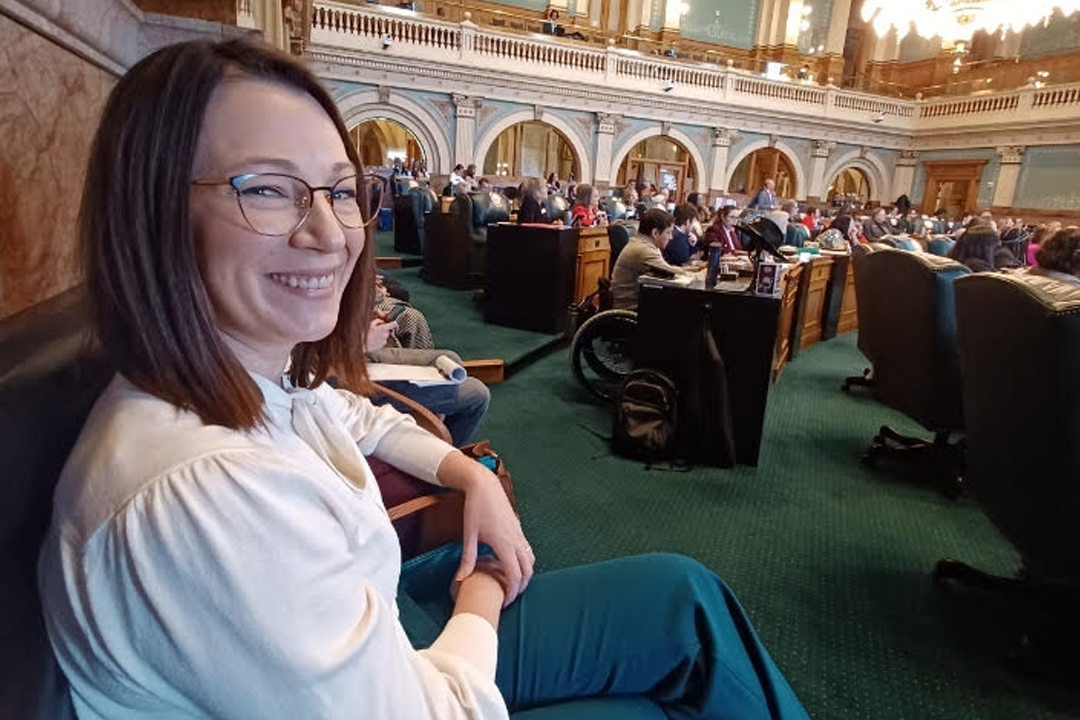
I started reaching out to legislators in the fall of 2022. It’s been an incredible process—I have had the chance to meet and engage with a wonderfully diverse group of individuals. My local collaborator is Liz Rosenbaum—she is a Colorado clean water activist who has been instrumental in helping me understand how the Colorado legislature works, inviting me to events to network and helping me navigate the capitol.
National advocacy groups including Compassion & Choices and Death with Dignity have been generous with their support and offering opportunities to educate and collaborate. I’ve also had the opportunity to collaborate with advocates from local organizations like Practically Dying and the Denver Health MAID clinic.
My advisors, Mary Jean Schumann and Dr. Mercedes Echevarria, and the faculty members in the Health Policy Program at GW have been phenomenal in providing practical advice and recommendations along the way. I would not have gotten this far without the support and encouragement from these wonderful individuals. I know we have more work to do, but we have a strong network that care about this issue that will work together for ongoing advocacy, which gives me hope.
Why is this legislation important to you?
This issue is important to me because patients deserve the right to choose what is best for them on their end-of-life journey. I know this is a sensitive topic and that it is not always easy to talk about death and dying. For those of us who choose to work with terminally ill individuals, though, conversations about what a dignified death looks like occur regularly. It is incredibly sad to listen to someone share their story about why the option of MAID is important to them and to ultimately watch the process of obtaining MAID fail or become excessively burdensome. The least I can do is share what this process really looks like for these individuals and to advocate on their behalf. My hope is that by sharing these concerns, that this will ultimately lead to a greater awareness of the challenges patients are facing and we can work towards adopting solutions that will benefit all Coloradans.